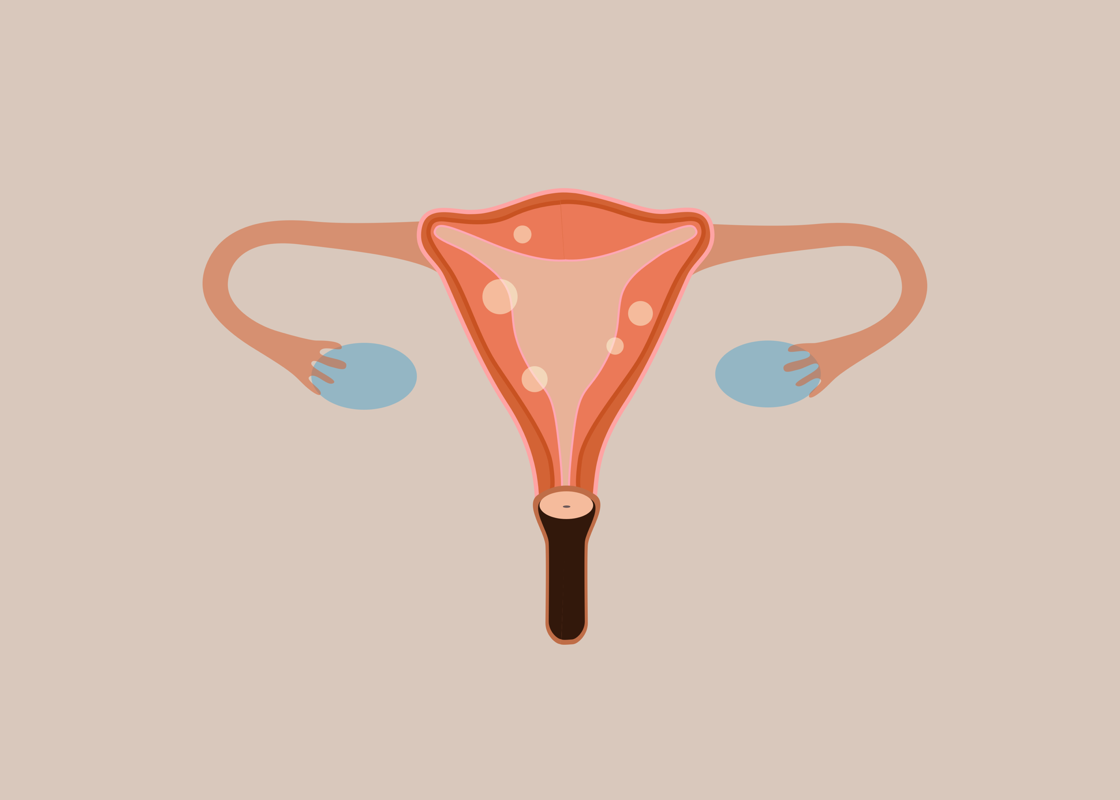
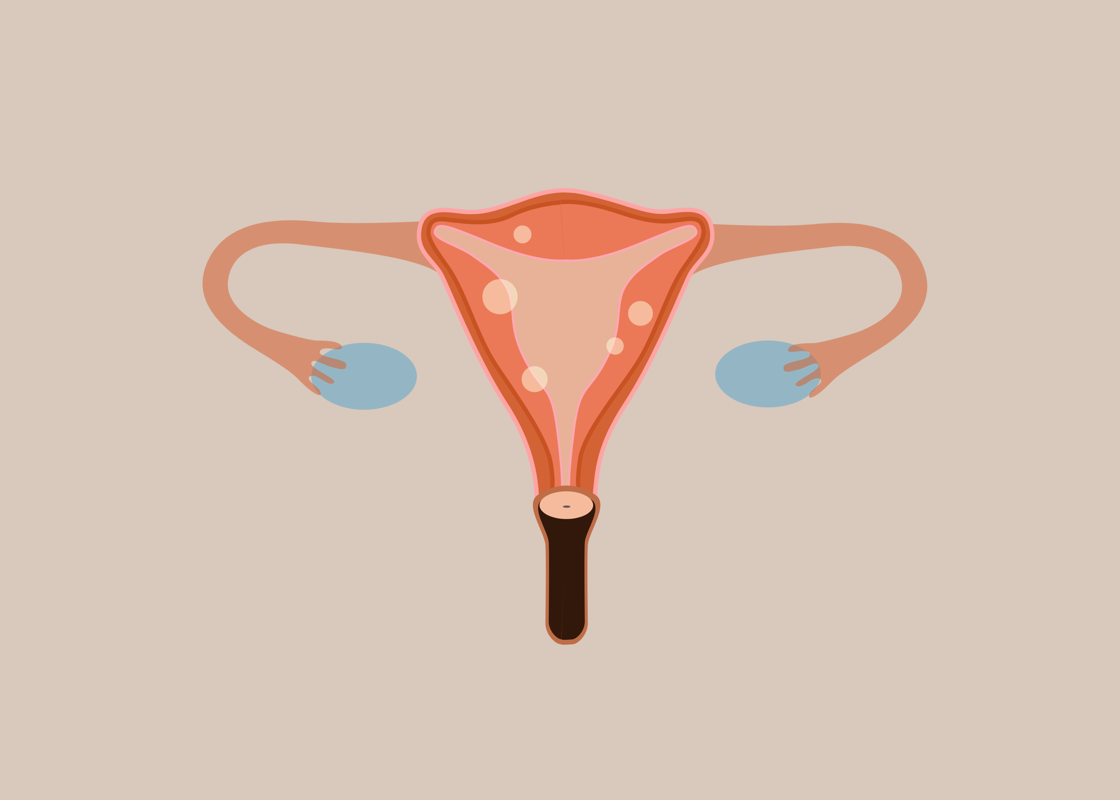
Did you know that uterine fibroids affect up to 80% of women? These are non-cancerous, smooth muscle tumors that grow either on, above, or outside of the uterus. They can exist without showing any signs. However, 30% of women will suffer symptoms of irregular menstrual cycles, anemia, painful intercourse, and fertility issues (1). Heavy bleeding caused by uterine fibroids can become debilitating, yet there is currently no preventative cure and only a vague understanding behind their root cause. Studies suggest that estrogen facilitates fibroids growth, and that after menopause, when the levels of estrogen lower in the body, fibroids can decrease in size (2). Ranging between being pea-sized, to growing as large as a melon, traditional medicine tends to only offer three options for treatment. These include the use of hormonal contraception to control estrogen levels, a surgical operation to cut the fibroids away or to have a hysterectomy.
Growing conversations about the alternative ways to manage uterine fibroids have led to women analysing how diet can impact the condition. This development sits in parallel with a fresh understanding of how psychosocial stress plays a significant role in the onset of their growth (3). Reports show that women of African ethnicity are three times more at risk of developing uterine fibroids (4). These worrying figures led us to investigate the condition further by speaking with Indi Allen. Indi has been diagnosed with fibroids twice in her life and offered to share with us her experience of the condition. Throughout this interview, Indi tells us about the symptoms she’s learnt to recognise. She also shares the holistic methods she turns to in order to manage her health.
I could feel these lumps sticking out of my belly and pulling with a pain that made me know something wasn’t normal.
Hello Indi, could you tell us what has shaped your approach to your female health today?
Looking back at my own education, it was really very basic. My mum was quite religious and strict, so sex and the body was something we didn’t talk about. I think this mindset came from her immigrant background and arriving in a country [the UK] with different ideas than what she had grown up around. We didn’t have things like sanitary towels. Instead, my mother would cut up cloth to use when bleeding. It was somewhat reflective of her own background due to my grandmother being one of the last generations to work on the British plantations as an indentured worker in Guyana, South America. This was a country that had a long history of slavery, and women’s health was a very taboo subject. This meant that, as a youngster, we never sat down to have a conversation about menstruation. What I learned was in biology class and that was it. I came to look at my own health later on in life when I became pregnant, and again when I started to have very heavy periods and fibroids.
What was your experience of pregnancy and how did you approach your self-care?
When I was first pregnant I went to the doctor and, even though I was looked after very well, I found everything became clinical very quickly. I think of other cultures, of my grandmother who gave birth upright in a field and see that the natural world can give us a lot of answers. I wanted to look after my own health this way. So I drank raspberry leaf tea, exercised, and took supplements. I had very low iron levels which I was prescribed tablets for. However, I wasn’t happy taking them; they made me constipated. Instead, I researched other options and found that by having orange juice and dark chocolate my iron levels went up. During labour I used arnica tablets and lavender oil. I also wanted to give birth standing up. The nurses were very disapproving of these ideas so I had to exert my authority over certain things. These conversations seem to be changing and it appears more common for women to take control of their own choices now. They have the option to have home births or water births.
You told us it was only after pregnancy that you started to have problems with your menstrual cycle. Could you tell us what changed?
It was ten years ago when I was in my early forties that things changed. I started to have very heavy bleeds which became almost impossible to manage, it was like a flood. I was very swollen in the stomach so I went to the doctor, they did some scans and diagnosed me with fibroids. One was growing on my ovary and I was told it could be cancerous therefore I would have to have a hysterectomy. I was really against that idea and instead, agreed to have surgery where they’d cut the fibroids away. I was given very little information about my condition at the time and felt like I didn’t have any options. I remember going in for my surgery, coming out of the operation and not remembering anything the surgeon told me post-op. They discharged me within the day. On the taxi ride home I felt so sick due to the anesthetic still being in my system. I wish I hadn’t left the hospital so soon because the recovery was horrendous. It took almost three years for me to get back to normal.
What helped you recover and how did your body change in the process?
For a long time, I felt like my core strength had been taken away. I could feel the scars and couldn’t press anything against my stomach. I was in big elasticated trousers and my body just didn’t feel right. I used oils, arnica creams, I did stretches and gave myself salt baths to try and help soothe the area. I felt mutilated due to the surgery, and my body took a long time to heal. Post-operation, I began having lots of skin problems and allergies. I don’t know if it was linked but my body started to become very sensitive to metal as well as other products so I started cutting things out of my life. I’m now in my fifties and 18 months ago, the fibroids came back. I could feel these lumps sticking out of my belly and pulling with a pain that made me know something wasn’t normal. This time around, the fibroids weren’t as big but the doctor told me the same thing as before: that I should use birth control to regulate my periods and then follow through with a full hysterectomy. I didn’t want either of these. Instead, I chose to take vitamins and supplements. For about three to four months I had very heavy periods then suddenly they stopped. This is something I have come to associate with being signs of menopause.
What methods of self-healing did you find helpful in managing your fibroids?
Exercise has been great and I’ve found that getting into patterns of looking after my body helped me. I run every day and regularly sea swim which has been fantastic. For me, it has been about enjoying whatever I do in regards to exercise. It is important to focus on your strength and what feels good rather than fixating on how your body has changed. They say massage is very good for fibroids so I use black seed oil when doing this which helps. My daughter, who was recently diagnosed with fibroids, is very hot on holistic healing. She advises me about what is good to eat and what I should avoid because food plays a really important role in regulating hormones. Sugar has been a big one because it can feed growths, so I try to stay away from refined sugars and incorporate natural alternatives into my diet. I think it goes back to looking at what your ancestors were eating. Using more basic diets that my grandmother grew up with and cutting out processed foods because they all contribute to our female health.
From your experiences, what do you think needs to change in regards to conversations surrounding fibroids?
We need to get the word out there. A wider group of women need to be able to look at their menstrual cycles, and conditions like fibroids and menopause more openly. We need more public information about the reality of women’s experiences. To share our stories with one another. Feeling my stomach for lumps has been a useful way of checking in with my health, and in general, I believe it’s all about education and self-awareness.
Disclaimer: Can you relate to Indi’s story? If you suspect anything abnormal, we suggest you approach your doctor.
References
-
Moro E, Degli Esposti E, Borghese G, et al. The Impact of Hormonal Replacement Treatment in Postmenopausal Women with Uterine Fibroids: A State-of-the-Art Review of the Literature. Medicina (Kaunas). 2019;55(9):549.
2. Borahay MA, Asoglu MR, Mas A, Adam S, Kilic GS, Al-Hendy A. Estrogen Receptors and Signaling in Fibroids: Role in Pathobiology and Therapeutic Implications. Reprod Sci. 2017;24(9):1235-1244.
3. Vines AI, Ta M, Esserman DA. The association between self-reported major life events and the presence of uterine fibroids. Women's Health Issues. 2010;20(4):294-298.
4. Catherino WH, Eltoukhi HM, Al-Hendy A. Racial and ethnic differences in the pathogenesis and clinical manifestations of uterine leiomyoma. Semin Reprod Med. 2013;31(5):370-379.